Targeted therapy for cancer is a modern treatment approach that focuses on the unique molecular changes driving a tumor’s growth. Instead of attacking healthy tissues, it zeroes in on specific genes, proteins, or pathways that fuel cancer development. This precision-based method has reshaped how patients experience treatment—offering hope through accuracy, reduced side effects, and personalized care. As advances in molecular testing expand, targeted therapy for cancer continues to open doors to more tailored and effective treatment journeys.
What is targeted therapy?
Targeted therapy for cancer refers to a specialized form of treatment designed to block the specific molecules that help cancer cells grow, divide, and spread. Unlike conventional treatments that affect both healthy and unhealthy cells, targeted drugs act with purpose, focusing only on the mechanisms that drive cancer progression. This approach allows for more personalized therapy because the treatment is chosen based on the patient’s tumor characteristics rather than a one-size-fits-all method.
Key points:
- Targets the root cause of cancer growth: Targeted therapy works by examining what makes a tumor behave abnormally—such as a mutated gene or overactive protein—and directly blocking that component. When these faulty pathways are shut off, cancer cells often lose their ability to multiply or survive.
- Designed for precision and personalization: Before starting treatment, doctors may perform genetic or molecular testing on the tumor to identify actionable mutations. This ensures that the targeted therapy is matched to the patient’s cancer profile, increasing the likelihood of response.
- Reduces unnecessary damage: By focusing on cancer-specific mechanisms, targeted therapy for cancer typically affects fewer healthy cells. This results in a treatment experience that may be gentler on the body while still effectively weakening cancer cells.
What are the types of targeted therapy?
There are several types of targeted therapy for cancer, each designed to interrupt cancer growth in different ways. These approaches are used across various cancers, including targeted therapy for breast cancer and other tumor types, depending on the molecular changes detected.
Key types:
- Monoclonal Antibodies: These lab-engineered molecules attach to specific proteins on the cancer cell surface. By binding to these targets, they can block growth signals or mark the cancer cells for destruction by the immune system. Many forms of targeted therapy for breast cancer use monoclonal antibodies to block HER2, a protein linked to aggressive tumor growth.
- Small Molecule Inhibitors: These drugs enter cancer cells and block abnormal signals within them. They are often used to shut down overactive growth pathways caused by mutations, such as EGFR or ALK in lung cancer. Their ability to work inside cells makes them powerful tools in targeted therapy for cancer treatment.
- Angiogenesis Inhibitors: These therapies stop tumors from forming new blood vessels. Without a steady supply of nutrients and oxygen, the tumor becomes weaker and may shrink over time. This approach is especially effective in cancers that heavily rely on rapid blood vessel formation.
Who is treated with targeted therapy?
Targeted therapy for cancer is typically recommended for individuals whose tumors carry specific mutations or biological markers that the treatment can act upon. Its use spans many cancer types, including targeted therapy for breast cancer and other solid tumors.
Key groups:
- Patients with identifiable gene mutations: Those whose tumors test positive for specific abnormalities—such as HER2, EGFR, ALK, or BRAF—are often the best candidates. These markers help determine whether the targeted therapy success rate is likely to be high for their cancer type.
- Patients who did not respond to standard therapy: When chemotherapy or radiation fails to control cancer, targeted therapy for cancer treatment can offer a more precise and effective alternative. It can also be combined with other treatments to improve outcomes in difficult-to-treat cases.
- Patients seeking personalized treatment approaches: Individuals looking for therapies with fewer side effects and more tailored action often benefit from targeted therapy. Because these treatments are chosen based on tumor biology, they provide a level of personalization that traditional methods cannot offer.
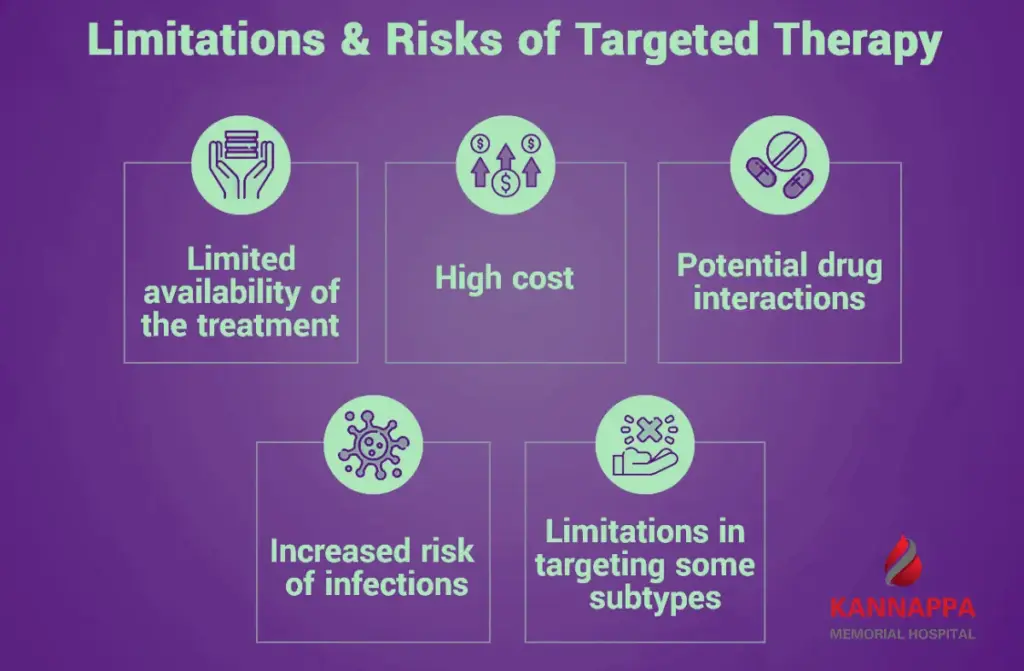
Are there drawbacks to targeted therapy?
While targeted therapy for cancer offers many advantages, it also comes with limitations. Its effectiveness often depends on finding a specific mutation, and not every tumor carries a treatable target.
Drawbacks:
- Cancer may develop resistance: Over time, tumors can adapt by changing or finding new pathways to grow. This resistance means that targeted therapy for cancer treatment might stop working, requiring a shift to another drug or combination approach.
- Limited to certain mutations: If a cancer does not have the required genetic mutation, targeted therapy may not be effective. This makes molecular testing essential and sometimes limits treatment options for patients without actionable markers.
- Potential side effects and high cost: Some targeted therapies can cause reactions like skin issues or fatigue. Additionally, many of these medications are expensive, which can make access challenging for some patients.
How does targeted therapy work against cancer?
Targeted therapy for cancer works by interrupting the specific processes that cancer cells rely on to survive. These drugs are designed to recognize and attack only those cells with certain genetic or protein abnormalities.
How it works:
- Blocking growth signals: Cancer cells often rely on overactive pathways that send constant signals to grow. Targeted therapy for breast cancer and other cancers can stop these signals, slowing or preventing tumor expansion.
- Triggering cancer cell death: Some targeted drugs interfere with proteins that cancer cells use for survival. When these proteins are blocked, the cancer cells lose their ability to repair or sustain themselves, leading to cell death.
- Preventing blood vessel formation: Tumors need new blood vessels to feed their growth. Drugs that block these signals starve the tumor of nutrients, making it harder for it to spread or grow.
What are targeted therapy benefits?
Targeted therapy for cancer brings several important benefits to patients seeking effective and personalized treatment options.
Benefits:
- Greater precision and fewer side effects: Because the drugs focus only on cancer-specific abnormalities, healthy cells are less affected. This increases comfort during treatment and improves quality of life during therapy.
- Positive targeted therapy success rate in selected patients: When a tumor has the right mutation, targeted therapy can produce strong and lasting responses. These results have made it a preferred option in many cancers with known genetic drivers.
- Personalized treatment approach: Targeted therapy allows clinicians to design a treatment plan based on the tumor’s molecular signature. This level of personalization helps guide better decisions and often leads to more predictable outcomes.
What are the side effects of targeted therapy?
Targeted therapy for cancer is known for being more selective than traditional treatments, yet it can still lead to certain reactions depending on how the drug interacts with cancer pathways.
Side effects:
- Skin and hair changes: Many targeted therapy side effects include rashes, dry skin, brittle nails, or hair thinning. These occur because some of the targeted pathways are also involved in skin cell growth and repair.
- Fatigue and digestive issues: Targeted therapy side effects may include tiredness, diarrhea, or mild nausea. These effects often arise when the drug impacts rapidly dividing cells in the digestive tract.
- High blood pressure and organ strain: Some drugs that block blood vessel formation may increase blood pressure or cause strain on organs like the liver. Close monitoring helps ensure these effects are managed early.
What can I expect when having targeted therapy?
When undergoing targeted therapy for cancer, patients typically experience a treatment process that is structured, monitored, and tailored to their needs.
What to expect:
- Comprehensive testing and evaluation: Your care team begins by performing molecular tests to identify the mutations driving your cancer. These results determine the medication best suited for you and help estimate the targeted therapy for cancer cost.
- Treatment through pills or infusions: Many targeted therapies are taken orally at home, while others are given through IV infusions. The schedule depends on the specific drug and your treatment plan.
- Regular monitoring: Doctors will track your response using scans, blood tests, and symptom checks. This close follow-up ensures the treatment remains effective and side effects are managed promptly.
How is targeted therapy different from chemotherapy?
Targeted therapy for cancer and chemotherapy work in very different ways, even though both aim to destroy cancer cells.
Differences:
- Precision vs. broad attack: Chemotherapy attacks all rapidly dividing cells, including some healthy tissues, whereas targeted therapy focuses on specific genetic or molecular traits of cancer cells. This makes targeted therapy for breast cancer and other cancers gentler on the body.
- Personalization: Chemotherapy doses are often based on factors like body size or cancer stage. Targeted therapy, however, is chosen only after understanding the tumor’s molecular features, making it a more individualized approach.
- Side effect profiles: Because chemotherapy affects many healthy tissues, side effects like hair loss, nausea, and low blood counts are common. Targeted therapy tends to avoid many of these issues, though it introduces different side effects linked to its mechanism of action.
Conclusion
Targeted therapy for cancer has transformed the landscape of modern cancer treatment by making care more precise, personal, and effective. Its ability to focus on the specific drivers of cancer not only improves outcomes but also minimizes unnecessary harm to healthy tissues. As research continues to uncover new targets, this approach will keep expanding treatment possibilities. If you or a loved one is navigating cancer care, exploring targeted options can open a pathway toward a more hopeful and tailored treatment journey.