Cord blood is the blood that remains in a baby’s umbilical cord and placenta after birth, carrying unique stem cells capable of restoring damaged blood and immune systems. These cells are often collected painlessly within minutes of delivery and stored for future therapeutic use. A cord blood transplant uses these powerful cells to treat life-threatening blood disorders, offering hope to patients who cannot find a matched bone marrow donor or need a faster treatment option.
What is a cord blood transplant?
A cord blood transplant is a treatment in which stem cells from a newborn’s umbilical cord are used to replace a patient’s diseased or damaged bone marrow. These stem cells can develop into healthy blood cells, helping the body recover from serious conditions like leukemia, lymphoma, or inherited blood disorders.
- The procedure begins with selecting a suitable cord blood unit stored in a public or private bank. Once infused, the stem cells travel to the patient’s bone marrow and begin forming new blood cells, gradually re-establishing immunity and healthy cell production.
- Cord blood requires less stringent genetic matching compared to bone marrow, making it accessible for patients who have struggled to find compatible donors. This flexibility allows treatment to move forward without long waiting periods.
- Because cord blood units are frozen and immediately available, they can be used quickly in medical emergencies. This is especially critical for rapidly progressing blood cancers, where delaying treatment could affect survival.
Types of Umbilical Cord Blood Banking
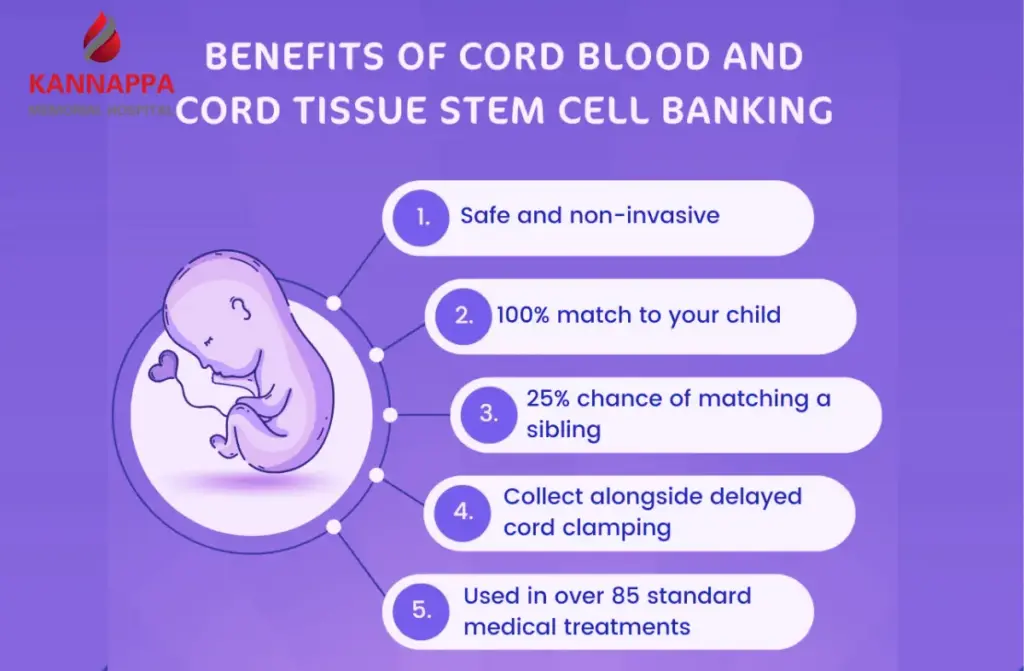
- Public Cord Blood Banking: Public banks store donated cord blood units that can be used by any patient requiring a cord blood transplant. These units undergo strict testing, processing, and cataloging to ensure they meet clinical standards. For families without financial means or those seeking to help others, public donation becomes a valuable contribution to umbilical cord blood transplant programs worldwide.
- Private Cord Blood Banking: Private banks store a newborn’s cord blood exclusively for the family’s future medical needs. This option appeals to parents who want a safety resource for conditions like immune deficiencies or inherited blood disorders. Although it is a paid service, it provides immediate access to stem cells genetically related to the child and potentially matched family members needing a cord blood bone marrow transplant.
- Hybrid or Community Banking Models: Some banks offer a shared-storage system where families pay lower fees in exchange for allowing their unit to be available for public use if needed. In such systems, the family can still access the cord blood if it has not been used for another patient. This approach balances affordability with a meaningful contribution to the global stem cell inventory.
Where does cord blood come from?
- Collected Immediately After Birth: Cord blood is obtained from the umbilical cord and placenta moments after delivery, once the baby is safely separated. The procedure is completely painless and takes place without disrupting any part of the childbirth experience. Because the collection is done quickly, it ensures the highest stem cell concentration for cord blood stem cell banking and transplantation.
- A Source of Young, Potent Stem Cells: The blood inside the cord contains hematopoietic stem cells, which can regenerate bone marrow after a cord blood transplant. These cells are biologically younger and adapt better to mismatches than adult bone marrow cells. Their flexibility makes them valuable in treatments such as a cord blood bone marrow transplant where donor compatibility may be limited.
- Safe to Collect and Store: Cord blood is collected using sterile methods and immediately transferred for processing. It is then frozen at extremely low temperatures and preserved for years. This stored unit remains ready for any future medical need related to cord blood stem cell banking and transplantation.
Who can have a cord blood transplant?
- Patients with Blood Cancers or Disorders: Individuals diagnosed with leukemia, lymphoma, myelodysplastic syndromes, or aplastic anemia often qualify for a cord blood transplant. These patients require complete replacement of diseased marrow to restore healthy blood production. Cord blood offers an option even when a full donor match cannot be found.
- Patients Without a Matched Donor: Many patients face challenges finding an HLA-matched bone marrow donor, especially those from mixed or underrepresented ethnic backgrounds. Cord blood relaxes matching requirements, allowing treatment to proceed sooner. In cases with low cell dose, a double cord blood transplant may be considered to provide adequate stem cells.
- Children and Certain Adult Patients: Cord blood is widely used in pediatric treatments due to the smaller cell dose required for children. Some adults also qualify, especially when medical teams determine that cord blood offers the safest or quickest pathway to transplant. When needed, two cord units are combined in a double cord blood transplant to ensure sufficient cell counts.
Benefits of cord blood
- Greater Flexibility in Matching: Cord blood requires less strict HLA matching compared to bone marrow, giving more patients access to treatment. This flexibility makes an umbilical cord blood transplant particularly valuable for ethnically diverse individuals who have difficulty finding donor matches. Faster matching improves treatment timelines for aggressive diseases.
- Lower Risk of Complications: Patients undergoing a cord blood transplant have a reduced risk of graft-versus-host disease due to the immature nature of cord cells. These cells are less likely to attack the patient’s tissues, providing a smoother recovery phase. This advantage is especially meaningful for patients already weakened by prior treatments.
- Readily Available Stem Cell Source: Cord blood units are stored frozen and can be used immediately. This eliminates delays often associated with donor searches and preparation for bone marrow donation. The rapid availability can significantly improve outcomes in time-sensitive conditions.
What will happen before the transplant?
- Pre-Transplant Evaluation: Patients undergo a detailed assessment to determine overall health, organ function, and disease status. Doctors review medical history, previous treatments, and suitability for a cord blood transplant. If cell dose is insufficient, a double cord blood transplant may be planned.
- Conditioning Treatment: Before receiving stem cells, patients undergo chemotherapy or radiation to eliminate diseased marrow. This conditioning also suppresses the immune system to allow the new cells to engraft successfully. The intensity of conditioning depends on the patient’s age, health, and diagnosis.
- Final Preparation and Support: The selected cord blood unit is thawed and prepared under sterile conditions. Patients may receive supportive care such as antibiotics or transfusions to stabilize them before infusion. Medical teams ensure that every detail is checked for safety and compatibility.
What will happen during the transplant?
- Infusion of Stem Cells: The thawed cord blood is infused through an IV line, similar to receiving a blood transfusion. The infusion is painless and typically takes a short time. This marks the beginning of the cord blood transplant process.
- Monitoring During Infusion: Clinical teams monitor vital signs, breathing, and patient comfort throughout the procedure. Any mild reactions, such as chills or flushing, are addressed immediately. Most patients tolerate the infusion well.
- Completion and Early Recovery: Once the infusion ends, the stem cells naturally move into the bone marrow spaces. They begin forming new blood cells over the following weeks. Supportive care continues to protect the patient from infections while the immune system rebuilds.
What will happen during the transplant?
- How the Stem Cells Work After Infusion: After completing the infusion, the cells migrate to the bone marrow where they begin engraftment. This critical phase is when the body starts producing new white cells, red cells, and platelets. The same process applies whether it is an umbilical cord blood transplant or a double cord blood transplant.
- Role of Stored Cord Blood Units: The cord blood used in the procedure comes from carefully preserved units collected through cord blood stem cell banking and transplantation programs. These units undergo strict quality checks before use. Whether for a cord blood bone marrow transplant or other conditions, the preserved stem cells are vital for recovery.
- Post-Procedure Care and Monitoring: Patients are closely watched for signs of engraftment, infections, or transplant-related complications. Doctors monitor blood counts and organ function daily until stability is observed. This careful oversight ensures that the cord blood transplant process proceeds safely and effectively.
Conclusion
A cord blood transplant has transformed treatment possibilities for patients with life-threatening blood disorders, offering hope when other donor options are limited. Its flexibility, rapid availability, and lower complication rates make it a powerful choice in modern medicine. If you or a loved one is exploring treatment paths, understanding the potential of cord blood may open new doors.
Speak with a qualified transplant specialist to assess whether this life-changing option is right for your condition.