Myelodysplastic Syndromes (MDS) are a group of rare but serious blood and bone marrow disorders. In MDS, the bone marrow—the spongy tissue inside bones that produces blood cells—fails to make enough healthy blood cells. Instead, it produces immature or abnormal cells that do not function properly. Over time, this leads to anemia, frequent infections, excessive bleeding, and, in some cases, progression to acute myeloid leukemia (AML). Once considered difficult to manage, MDS is now better understood thanks to advances in genetics and treatment research. Although it most commonly affects older adults, anyone can be diagnosed. Early recognition, precise diagnosis, and tailored treatment are essential to improving outcomes.
MDS is classified as a type of bone marrow failure disorder. In healthy individuals, bone marrow produces:
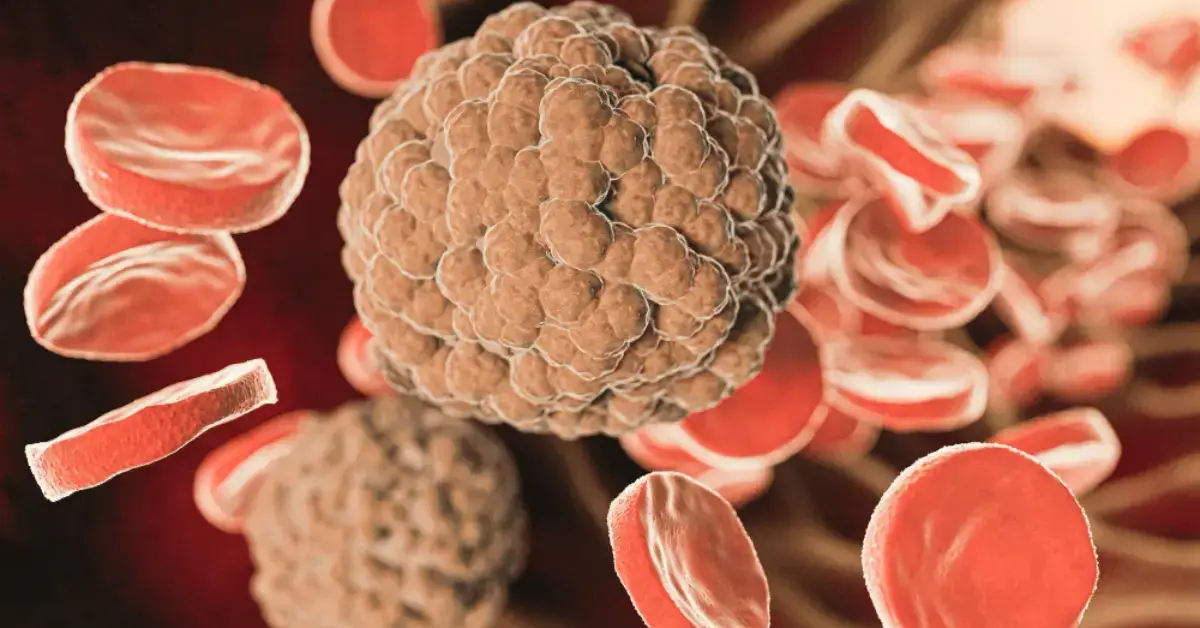
In MDS, abnormal stem cells in the bone marrow create defective blood cells. These immature cells die earlier than normal, leaving fewer healthy cells in circulation. This condition is sometimes called “pre-leukemia” because of its potential to progress to acute myeloid leukemia.
The World Health Organization (WHO) classifies MDS into several subtypes based on blood cell appearance and genetic changes:
MDS arises when bone marrow stem cells acquire genetic mutations. While the exact cause is not always clear, risk factors include:
Many patients are asymptomatic in early stages, and the condition is often discovered during routine blood tests. Common symptoms include:
Because symptoms overlap with other illnesses, early medical evaluation is critical.
Doctors use a combination of tests to confirm MDS:
Diagnosis also includes risk stratification, using scoring systems like:
These tools assess survival chances and progression risk to AML.
The choice of treatment depends on age, health, risk category, and subtype. Treatments are often divided into supportive care, disease-modifying therapies, and curative options.
Managing MDS requires not just medical treatment but also lifestyle adjustments:
Recent breakthroughs have transformed MDS management:
MDS prognosis varies widely:
Survival depends on:
With ongoing research, survival rates are improving, and patients now have more options than ever before.
Myelodysplastic Syndromes are complex blood disorders that demand accurate diagnosis, personalized treatment, and long-term care. While there is currently no universal cure, therapies such as stem cell transplantation and hypomethylating agents are offering patients better survival and quality of life.
Early detection and active disease monitoring are essential in improving outcomes. Raising awareness of MDS ensures that more people recognize the symptoms early and seek timely medical attention. With rapid advances in research, the future holds greater hope for patients and families affected by MDS.
Myelodysplastic Syndromes (MDS) are a group of rare but serious blood and bone marrow disorders. In MDS, the bone marrow—the spongy tissue inside bones that produces blood cells—fails to make enough healthy blood cells. Instead, it produces immature or abnormal cells that do not function properly. Over time, this leads to anemia, frequent infections, excessive bleeding, and, in some cases, progression to acute myeloid leukemia (AML). Once considered difficult to manage, MDS is now better understood thanks to advances in genetics and treatment research. Although it most commonly affects older adults, anyone can be diagnosed. Early recognition, precise diagnosis, and tailored treatment are essential to improving outcomes.
What is Myelodysplastic Syndrome (MDS)?
Types of MDS
Causes and Risk Factors
Symptoms of MDS
Diagnosis of Myelodysplastic Syndromes
Treatment Options for MDS
Living with MDS
Advances in Research
Prognosis and Outlook
Conclusion
MDS is classified as a type of bone marrow failure disorder. In healthy individuals, bone marrow produces:
In MDS, abnormal stem cells in the bone marrow create defective blood cells. These immature cells die earlier than normal, leaving fewer healthy cells in circulation. This condition is sometimes called “pre-leukemia” because of its potential to progress to acute myeloid leukemia.
The World Health Organization (WHO) classifies MDS into several subtypes based on blood cell appearance and genetic changes:
MDS arises when bone marrow stem cells acquire genetic mutations. While the exact cause is not always clear, risk factors include:
Many patients are asymptomatic in early stages, and the condition is often discovered during routine blood tests. Common symptoms include:
Because symptoms overlap with other illnesses, early medical evaluation is critical.
Doctors use a combination of tests to confirm MDS:
Diagnosis also includes risk stratification, using scoring systems like:
These tools assess survival chances and progression risk to AML.
The choice of treatment depends on age, health, risk category, and subtype. Treatments are often divided into supportive care, disease-modifying therapies, and curative options.
Managing MDS requires not just medical treatment but also lifestyle adjustments:
Recent breakthroughs have transformed MDS management:
MDS prognosis varies widely:
Survival depends on:
With ongoing research, survival rates are improving, and patients now have more options than ever before.
Myelodysplastic Syndromes are complex blood disorders that demand accurate diagnosis, personalized treatment, and long-term care. While there is currently no universal cure, therapies such as stem cell transplantation and hypomethylating agents are offering patients better survival and quality of life.
Early detection and active disease monitoring are essential in improving outcomes. Raising awareness of MDS ensures that more people recognize the symptoms early and seek timely medical attention. With rapid advances in research, the future holds greater hope for patients and families affected by MDS.
Myelodysplastic syndrome (MDS) is a group of disorders where the bone marrow does not produce enough healthy blood cells. Instead, it makes immature or abnormal cells that cannot function properly. This leads to anemia, infections, or bleeding issues. MDS is sometimes called a “bone marrow failure disorder” and may progress into acute myeloid leukemia in severe cases.
The four main types of myelodysplastic syndrome include refractory anemia (RA), refractory anemia with ring sideroblasts (RARS), refractory anemia with excess blasts (RAEB), and chronic myelomonocytic leukemia (CMML). Each type is classified based on abnormal cell development in bone marrow and blood, severity of symptoms, and risk of progression to acute leukemia. Proper diagnosis guides treatment options.
Life expectancy in myelodysplastic syndrome varies depending on the type, age, and treatment response. Some low-risk cases progress slowly, allowing patients to live for years with proper management, while high-risk cases may advance quickly to leukemia. On average, survival ranges from less than a year to over a decade. Advances in treatments continue to improve outcomes.