A bone marrow transplant is a life-saving medical procedure where damaged or diseased bone marrow is replaced with healthy stem cells. This treatment is often used for patients battling blood cancers like leukemia or disorders like aplastic anemia. It offers hope where conventional therapies fall short, helping the body regenerate healthy blood cells. As promising as it is, several factors affecting bone marrow transplant cost such as donor type, hospital stay, and post-treatment care can influence the overall treatment journey. Understanding its process and advantages is key before making informed decisions.
What is a Bone Marrow Transplant?
A bone marrow transplant is a medical procedure that replaces damaged or diseased bone marrow with healthy stem cells to restore normal blood cell production. It is often used to treat cancers like leukemia, lymphoma, and multiple myeloma, as well as severe anemia or immune disorders. The Bone Marrow Transplant Treatment Cost Explained varies based on transplant type autologous (self-donor) or allogeneic (donor) and hospital expertise. Key Factors Affecting Bone Marrow Transplant Cost include diagnostic tests, donor matching, hospitalization duration, post-transplant medications, and ongoing monitoring. Understanding these aspects helps patients prepare both medically and financially for this complex yet life-saving procedure, ensuring transparency and informed decision-making throughout the treatment process.
Why is it Needed?
A bone marrow transplant becomes essential when the body’s natural ability to produce healthy blood cells is compromised or entirely damaged. This life-saving procedure is often recommended for individuals with serious blood-related conditions where standard treatments are no longer effective. Knowing what influences bone marrow transplant cost starts with understanding the medical urgency behind it and the Factors Affecting Bone Marrow Transplant Cost.
- Replacement of Faulty Bone Marrow: Diseases like aplastic anemia lead to the complete failure of bone marrow, making it impossible for the body to generate red cells, white cells, or platelets. Transplantation becomes the only route to restore vital blood production and avoid chronic transfusions or infections.
- Treatment for Blood Cancers and Disorders: Bone marrow transplants are commonly used to treat cancers such as leukemia, lymphoma, and multiple myeloma. These diseases interfere with normal blood cell production, and a transplant offers a way to replace the damaged marrow with healthy, functioning cells.
- Support for Genetic and Immune System Disorders: Conditions like thalassemia, sickle cell anemia, and certain immunodeficiencies may require a bone marrow transplant to restore the body’s ability to fight infections and maintain healthy blood cell levels. Without this intervention, patients may experience life-threatening complications over time.
- Recovery After High-Dose Chemotherapy or Radiation: In aggressive cancer treatments, the bone marrow often becomes severely weakened or destroyed. A transplant helps rebuild the blood-forming system, allowing the patient to recover and regain immunity and strength.
Who Needs it? – Comparison
Bone marrow transplants are not limited to a single condition or age group. Patients of various backgrounds, with different medical diagnoses and health statuses, may require this procedure based on the severity of their illness and how well they respond to initial treatments. The table below outlines key patient categories who may need a bone marrow transplant and how their individual situations relate to what influences bone marrow transplant cost.
| Patient Type | Medical Condition | Why Transplant is Required | What Influences Bone Marrow Transplant Cost |
| Children with Genetic Disorders | Thalassemia, Sickle Cell Anemia, Immunodeficiencies | Their bone marrow cannot produce healthy blood cells due to inherited conditions, requiring replacement to ensure long-term survival. | Cost varies based on donor matching complexity, pre-transplant care, and prolonged pediatric ICU monitoring. |
| Adults with Blood Cancers | Leukemia, Lymphoma, Multiple Myeloma | High-dose chemotherapy or radiation damages marrow; transplant restores ability to form healthy blood cells. | Influenced by cancer stage, treatment cycles before transplant, and need for specialized oncology support. |
| Patients with Bone Marrow Failure | Aplastic Anemia, Myelodysplastic Syndromes | Their bone marrow is non-functional or severely underperforming; transplant becomes necessary for blood regeneration. | Depends on diagnostic tests, type of transplant (autologous or allogeneic), and extended hospital stays due to complications. |
| Relapsed Cancer Patients | Cancer returning after initial remission | When other treatments fail or disease returns, a transplant may offer the only chance for recovery. | Costs rise with repeated treatments, multiple donor searches, and post-transplant surveillance. |
| Patients with Autoimmune Conditions | Severe Systemic Lupus Erythematosus, Multiple Sclerosis (in clinical settings) | In rare cases, transplant is used to reset the immune system in treatment-resistant autoimmune diseases. | Influenced by experimental nature of the treatment, need for long-term immunosuppression, and specialized care settings. |
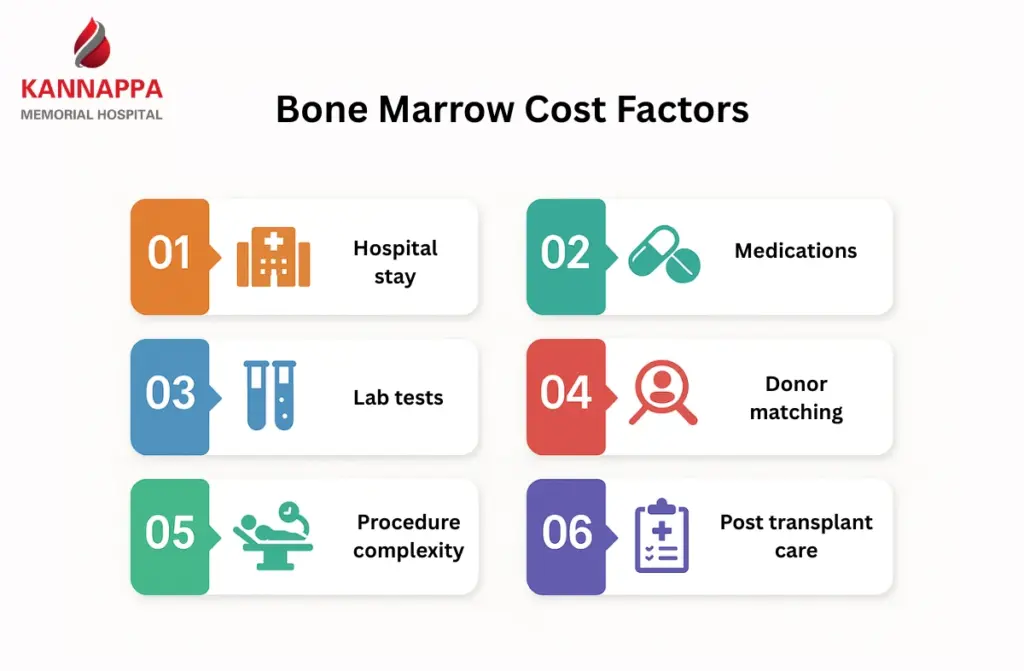
Cost Influencing Factors
Understanding the factors affecting bone marrow transplant cost is crucial for patients and families planning treatment. Several medical, logistical, and personal considerations contribute to the overall expense, and each factor can significantly alter the financial requirements of the procedure.
- Donor Matching and Source: Costs can rise significantly if a matched donor is not available within the family and needs to be found through national or international registries.
- Pre-Transplant Evaluation and Conditioning: Extensive testing, imaging, and chemotherapy or radiation are often required before the transplant to prepare the body. These pre-conditioning treatments vary in intensity based on the patient’s health and diagnosis, directly influencing the cost structure.
- Hospital Stay and ICU Monitoring: Bone marrow transplants often require a prolonged hospital stay, especially during the immune-compromised phase post-transplant. The need for isolation units, specialized nursing care, and ICU support in case of complications contributes to higher hospitalization expenses.
- Post-Transplant Complications and Recovery: Graft-versus-host disease (GVHD), infections, and delayed engraftment may require advanced treatment and extended care. The longer and more intensive the recovery phase, the higher the financial burden due to additional medications, transfusions, and specialist consultations.
- Supportive Medications and Immunosuppressants: After the transplant, patients are prescribed costly medications to prevent rejection and manage side effects. These drugs may be needed for several months to years, significantly adding to the cumulative cost over time.
Types of Bone Marrow Transplants
Here’s a concise breakdown of each marrow transplant type, with bone marrow transplant treatment cost explained through their unique medical and financial considerations:
- Autologous Transplant (Self-Donor): Uses the patient’s own stem cells, making it lower in cost and risk of rejection. However, there’s a chance of reintroducing cancer cells.
- Allogeneic Transplant (Donor-Based): Uses cells from a matched donor, ideal for genetic or severe marrow disorders. Costs are higher due to donor matching and post-transplant care.
- Haploidentical Transplant (Half-Matched Donor): Involves a partially matched family member, expanding donor options. It requires advanced care, raising the treatment expense.
Factors Affecting Bone Marrow Transplant Cost in India
The cost of a bone marrow transplant in India can vary widely due to a combination of medical, logistical, and institutional factors. Each stage of the procedure from donor matching and pre-transplant evaluations to the actual transplant and post-procedure care requires specialized expertise, advanced technology, and extensive resources. Understanding these factors not only helps patients plan financially but also enables them to choose the most suitable treatment approach based on their medical needs and budget.
- Type of transplant and donor source: Autologous, allogeneic, and cord blood transplants differ substantially in complexity and resource needs; allogeneic transplants especially from unrelated or partially matched donors require extensive donor search, graft processing and immunological monitoring, which raises costs. The stem cell source (peripheral blood, bone marrow, cord blood) also affects collection procedures and laboratory handling fees.
- Pre-transplant evaluation and conditioning regimen: Comprehensive pre-transplant workup including HLA typing, infectious disease screening, cardiac and pulmonary assessments, and specialized imaging contributes to upfront expenses and helps determine risk stratification. Myeloablative conditioning with high-dose chemotherapy or total body irradiation increases drug, inpatient and supportive care costs compared with reduced-intensity regimens.
- Hospital stay length and level of care: Prolonged inpatient stays, isolation facilities and ICU admissions drive daily room charges, advanced nursing care and consumable use, making hospitalization a major cost component. Use of specialized services such as stem cell processing labs and the range of Laboratory Services & Diagnostics and Critical Care & Inpatient Services further increases institutional fees.
- Post-transplant medications and complication management: Long-term immunosuppressants, antimicrobial prophylaxis, growth factors and transfusions are recurring cost drivers, and treating complications such as graft-versus-host disease or severe infections can require costly biologics and extended hospitalisation. Frequent outpatient monitoring, repeat investigations and possible readmissions must be factored into the total expense.
- Institutional, regional and insurance factors: Leading transplant centres with multidisciplinary teams and accreditations may charge higher fees, while prices vary between metropolitan and smaller-city hospitals due to differences in overhead and supply costs. The extent of insurance coverage, government schemes or negotiated package rates greatly influences out-of-pocket expenditure, so net cost depends heavily on available financial protection.
Why Choose Us?
At Kannapa Hospital, our approach to bone marrow transplantation blends clinical precision with compassionate care. We are committed to making advanced treatment accessible while offering transparency through our detailed Bone Marrow Transplant Cost Guide, which outlines the key Factors Affecting Bone Marrow Transplant Cost such as treatment type, donor matching, hospital stay, and post-transplant care. This ensures patients and families can navigate this critical phase with clarity, confidence, and continuous support.
- Expertise in High-Risk Transplants: Our transplant team includes hematologists, oncologists, and immunologists with extensive experience in handling both autologous and complex allogeneic transplants. Their multidisciplinary approach ensures each case is evaluated thoroughly, optimizing outcomes and minimizing complications.
- Advanced Infrastructure and Safety Protocols: The hospital is equipped with HEPA-filtered transplant units, specialized isolation rooms, and 24/7 critical care support. These safety-focused facilities reduce infection risk and allow us to handle immunocompromised patients with the highest level of precision and hygiene.
- Ethical Cost Transparency: We follow a structured, patient-friendly bone marrow transplant cost guide that outlines all stages of treatment. From donor evaluation to post-discharge follow-ups, patients receive clear cost estimates, helping them plan without unexpected expenses.
- Post-Transplant Monitoring and Recovery: Kannapa Hospital prioritizes long-term recovery with dedicated post-transplant clinics. Patients benefit from regular follow-ups, personalized medication plans, nutritional guidance, and psychological support ensuring continuity of care even after discharge.
- Access to a Diverse Donor Network: Our affiliations with national and international donor registries improve the chances of finding suitable matches. This greatly benefits patients without familial donors and enables quicker transplant timelines without compromising match quality.
- Integrated Patient Support Services: From financial counseling to assistance with insurance documentation, we provide non-clinical services that ease the overall journey. Families receive continuous updates, counseling, and logistical help, allowing them to focus solely on recovery.
Conclusion
Navigating the journey of a bone marrow transplant involves making crucial medical and financial decisions. By understanding the factors affecting bone marrow transplant cost, patients and caregivers can plan their treatment with greater confidence. Elements such as donor matching, hospital type, medication duration, and post-operative care all play significant roles. At Kannapa Hospital, we offer a patient-first approach with clear financial pathways to support recovery. Our goal is to deliver life-saving care without compromising transparency or trust.